Lub-dub. Lub-dub. A healthy heart beats at regular intervals, an action which pushes blood smoothly through its chambers and into the body. If your heart’s electrical signals aren’t working properly, however, it can interrupt that steady rhythm.
The most common form of abnormal heart rhythm is atrial fibrillation (AFib), a condition in which the heart’s upper chambers beat erratically. AFib has potentially serious health implications. Typical symptoms include heart palpitations, shortness of breath, dizziness and chest pain, all of which can intrude upon daily life. That may not even be the most frightening part: People with AFib face a higher risk of heart failure and dementia, as well as a five-fold increase in their risk of stroke.
The first line of defense against AFib is usually medications like antiarrhythmics and anticoagulants (blood thinners), but each has side effects that can make it difficult to tolerate long-term. And then there’s another highly effective option for AFib treatment: cardiac ablation. This minimally invasive procedure is designed to deliver a blast of energy to misbehaving cardiac cells, rebooting the heart’s electrical circuitry and bringing its rhythm back to normal.
There are two different approaches to cardiac ablation for AFib: traditional thermal ablation, and a newer method called pulsed field ablation.
Thermal ablation for AFib
The traditional form of cardiac ablation is called thermal ablation, which uses hot or cold energy to either burn or freeze the malfunctioning heart cells. Here’s how it’s done: While a person is under anesthesia, a skilled physician snakes a thin, flexible tube called a catheter through the groin, up through a vein leading to the heart, and into the heart’s top left chamber.
If hot energy is being used (radiofrequency ablation), the catheter transfers energy to the targeted cardiac cells, heating them to a high temperature. If cold energy is being used (cryoablation), the doctor moves a tiny balloon out from the end of the catheter, inflates it, nestles it precisely into the junction where the pulmonary vein meets the upper left chamber of the heart, then delivers an icy shock to the targeted cells. Because precision is important, it’s helpful for doctors to have tools that can adapt to different patient anatomies.
In both types of thermal ablations, the energy kills misbehaving cells and creates tiny scars to disable any further abnormal electrical rhythms from being conducted. The procedures typically take a little over an hour and are highly effective for treating AFib.
While these products have been proven safe and effective, thermal ablation – like any medical procedure – does carry risks. Just to the other side of the pulmonary vein are nerve and muscle cells that can inadvertently get a dose of that thermal energy blast, potentially resulting in injury to the esophagus, nerve damage or a narrowing of the pulmonary vein (pulmonary stenosis). This is where pulsed field ablation (PFA) is showing tremendous promise in reducing or even eliminating these risks.
Pulsed field ablation for AFib treatment
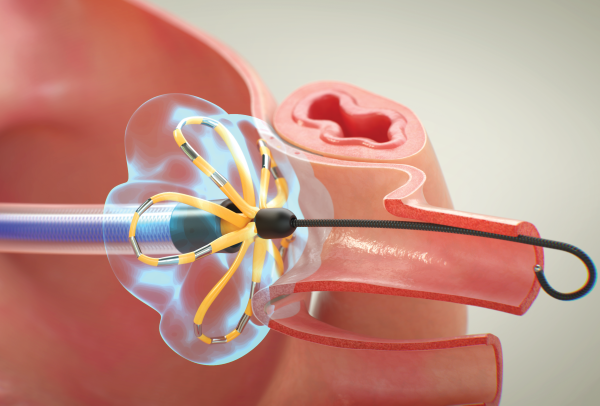
Instead of using thermal energy, PFA uses high-output electrical signals that isolate specific heart cells, causing them to split and die in a precise pattern. These signals are delivered via catheter rather than by inflatable balloon.
In the FARAPULSE™ Pulsed Field Ablation System, the catheter first assumes a rounded “basket” shape, which a physician nestles into a precise position at the pulmonary vein. After applying short bursts of energy, the physician pulls the catheter back to flatten the basket, creating a unique, looping flower shape. The flexible “petals” of that flower are then placed against the entrance of the pulmonary vein for a few final beams of energy to finish off the procedure.
Those changes have led to impressive results for AFib patients. Clinical data has shown FARAPULSE to be as safe and effective as thermal alternatives, with procedure times that are significantly shorter – results that have been echoed by extensive, real-world data from around the globe. What’s more, clinical evidence shows that the FARAPULSE procedure results in fewer unwanted side effects.
“We haven’t seen esophageal injury or pulmonary vein stenosis in nearly 40,000 cases conducted commercially or in any of our clinical trials,” says Brad Sutton, M.D., chief medical officer of atrial fibrillation solutions at Boston Scientific. “Such strong safety and efficacy outcomes make this an exciting development for physicians.” Watch FARAPULSE in action in this video:
With the addition of FARAPULSE, Boston Scientific has one more important tool in the cardiac ablation toolbox, allowing physicians to make a more informed AFib treatment decision for each individual patient.
Learn more about how pulsed field ablation works to treat AFib (atrial fibrillation).
***This story was updated on January 22, 2026.