Building a better stroke-risk reduction device: the WATCHMAN FLX™ Pro Left Atrial Appendage Closure Implant
As many as 6 million people in the United States have atrial fibrillation (AFib) – a condition in which the heart beats erratically. And their diagnosis means there’s always a second shoe threatening to drop: Living with AFib puts patients at a five-fold greater risk of stroke.
The first-line treatment for AFib is oral anticoagulant (a.k.a. blood-thinning) medication. These drugs do have a downside, however – they can increase bleeding risk.
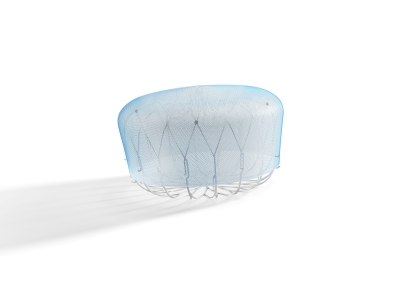
Enter the WATCHMANTM Left Atrial Appendage Closure (LAAC) Device, which is implanted through a minimally invasive procedure to close off the left atrial appendage (LAA) of the heart where clots are especially prone to forming. The WATCHMAN LAAC device was first introduced to the European market in 2009. In 2015, it became the first device approved by the U.S. Food and Drug Administration (FDA) for use in the LAA to reduce stroke risk in people who have nonvalvular AFib, a form of AFib that isn’t caused by a heart valve issue.
The WATCHMAN FLX™ LAAC Device, approved by the FDA in 2020, then built upon the original technology by making the procedure safer, more efficient and creating improved clinical outcomes.
Today, more than 300,000 patients have been treated with the WATCHMAN therapy globally, and it’s been proven safe and effective through numerous randomized clinical trials and real-world studies.
More controlled healing and reduced risk of device-related blood clots
Our R&D teams continue to explore new ways to fine-tune and improve the device based on what is learned through clinical research and real-world clinical practice.
“We listen really closely to our physician advisors, and they identified a couple of remaining unmet needs with the product,” says Dr. Brad Sutton, chief medical officer for our AFib Solutions business at Boston Scientific.
One such unmet need was a way to reduce the risk of device-related thrombus (DRT), the term used to describe blood clots that can potentially form on medical devices, including those that are used to treat cardiovascular diseases. In the case of the WATCHMAN FLX technology, the risk of DRT was very low but still possible in rare instances.
The suggestion led to the evaluation of dozens of materials and coatings that might be used on the product exterior to help further reduce this risk, and potentially promote faster, more complete healing around the device at the same time. Ultimately, the WATCHMAN R&D team selected a thromboresistant polymer coating that has a long history of safe use on other implantable medical devices.
Preclinical research of the polymer coating bears this out, showing that it provided an 86% reduction in inflammation of the coated WATCHMAN device three days following implantation and a 70% reduction of thrombus at 14 days. This innovative technology will soon be in reach for people with non-valvular AFib as part of the new WATCHMAN FLX TM Pro device, which was just approved for use by the FDA.
Because the WATCHMAN FLX Pro is designed to provide faster, more controlled healing after implantation in addition to a stroke reduction benefit, it’s possible that patients could one day require a less aggressive drug regimen than the one they currently need to take post implant, Dr. Sutton says.
The device also features new radiopaque visualization markers to help physicians place it more precisely, as well as a new size expanding the treatable patient population to those patients with larger left atrial appendages.
“The anatomy of the LAA is very complex,” explains Mathew Gilk, vice president, Research and Development (R&D) and Program Management, Boston Scientific. “People liken it to a fingerprint – it’s that unique to each individual. So there’s a range of sizes and configurations that need to be accommodated.”
Reaching new patients while continuing to refine
Prior to FDA approval, the WATCHMAN FLX Pro device was only available to people with AFib who are part of the ongoing WATCHMAN FLX Pro CT single-center study, which is tracking healing in the form of tissue coverage around the device after implantation.
Now that the device is FDA-approved, the WATCHMAN FLX Pro device will be evaluated in approximately 1,000 patients at 60 sites across the U.S. through the HEAL-LAA study to assess real-world clinical outcomes after receiving the device.
The new technology is expected to reach additional patients with nonvalvular AFib who qualify for the therapy beginning in 2024.
What all these patients have in common is the security of receiving a device that’s been built on years of safety and performance evidence collected through the previous two generations of the WATCHMAN therapy.
“Not many devices that I can think of have the volume of real-world data that we have around the WATCHMAN procedure,” says Gilk. “It’s an incredible achievement to see that level of consistency in clinical outcomes over time.”
Learn more about the newly FDA-approved WATCHMAN FLX Pro therapy.